
A SOP Template for Medical Billing Services provides a standardized framework to ensure accuracy and compliance in processing healthcare claims. It outlines step-by-step procedures for verifying patient information, coding medical services, and submitting claims to insurance providers. This template enhances efficiency and reduces errors, improving the overall revenue cycle management in medical practices.
Client onboarding and documentation verification.
This SOP describes the process for client onboarding and documentation verification, including initial client information collection, identity and document validation, compliance with regulatory requirements, data entry into the system, and confirmation of client acceptance. The purpose is to ensure a seamless onboarding experience while maintaining accuracy, security, and adherence to legal standards.
Patient demographics entry and account creation.
This SOP details the process for accurate patient demographics entry and account creation, encompassing the collection, verification, and input of essential patient information, including personal details, contact information, insurance data, and emergency contacts. The goal is to ensure the integrity and confidentiality of patient records while facilitating efficient account setup for seamless healthcare service delivery and billing processes.
Insurance verification and eligibility checks.
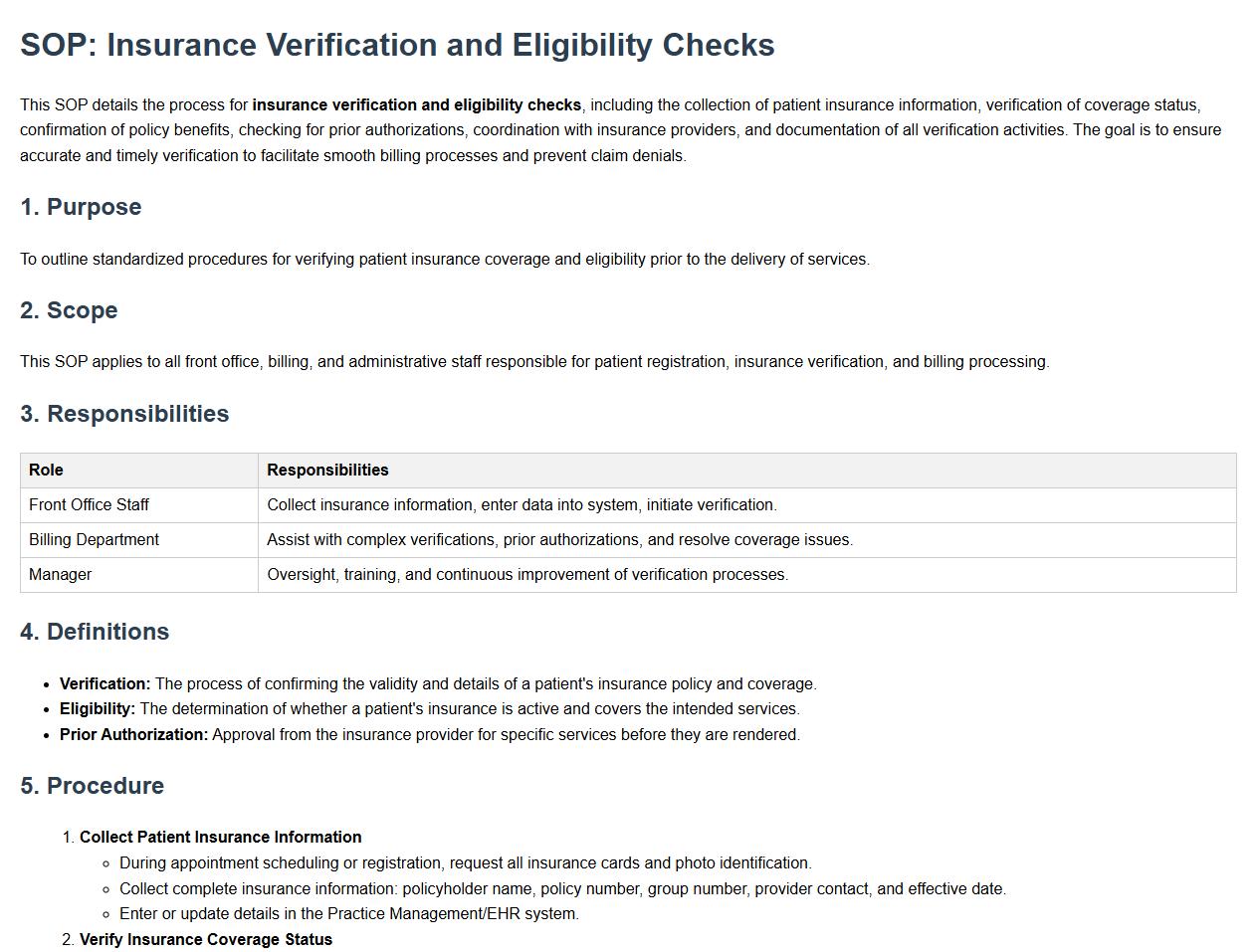
This SOP details the process for insurance verification and eligibility checks, including the collection of patient insurance information, verification of coverage status, confirmation of policy benefits, checking for prior authorizations, coordination with insurance providers, and documentation of all verification activities. The goal is to ensure accurate and timely verification to facilitate smooth billing processes and prevent claim denials.
Charge entry and coding compliance procedures.
This SOP details charge entry and coding compliance procedures, encompassing accurate charge documentation, proper medical coding practices, verification of billing information, adherence to regulatory and payer requirements, timely charge submission, audit readiness, and corrective action protocols. The goal is to ensure billing accuracy, maximize reimbursement, and maintain compliance with healthcare regulations.
Claims generation, submission, and tracking.
This SOP details the process for claims generation, submission, and tracking, including accurate claim preparation, timely submission to relevant entities, monitoring claim status, managing discrepancies or denials, and maintaining comprehensive documentation. The goal is to streamline the claims lifecycle to ensure efficient reimbursement, minimize errors, and support effective communication between all stakeholders involved in the claims management process.
Payment posting and reconciliation process.
This SOP details the payment posting and reconciliation process, encompassing procedures for accurately recording incoming payments, matching payments to outstanding invoices, managing discrepancies, updating financial records, and ensuring the integrity of accounts receivable. It aims to streamline payment processing, maintain accurate financial data, and facilitate timely reconciliation to support effective financial management and reporting.
Denial management and appeals workflow.
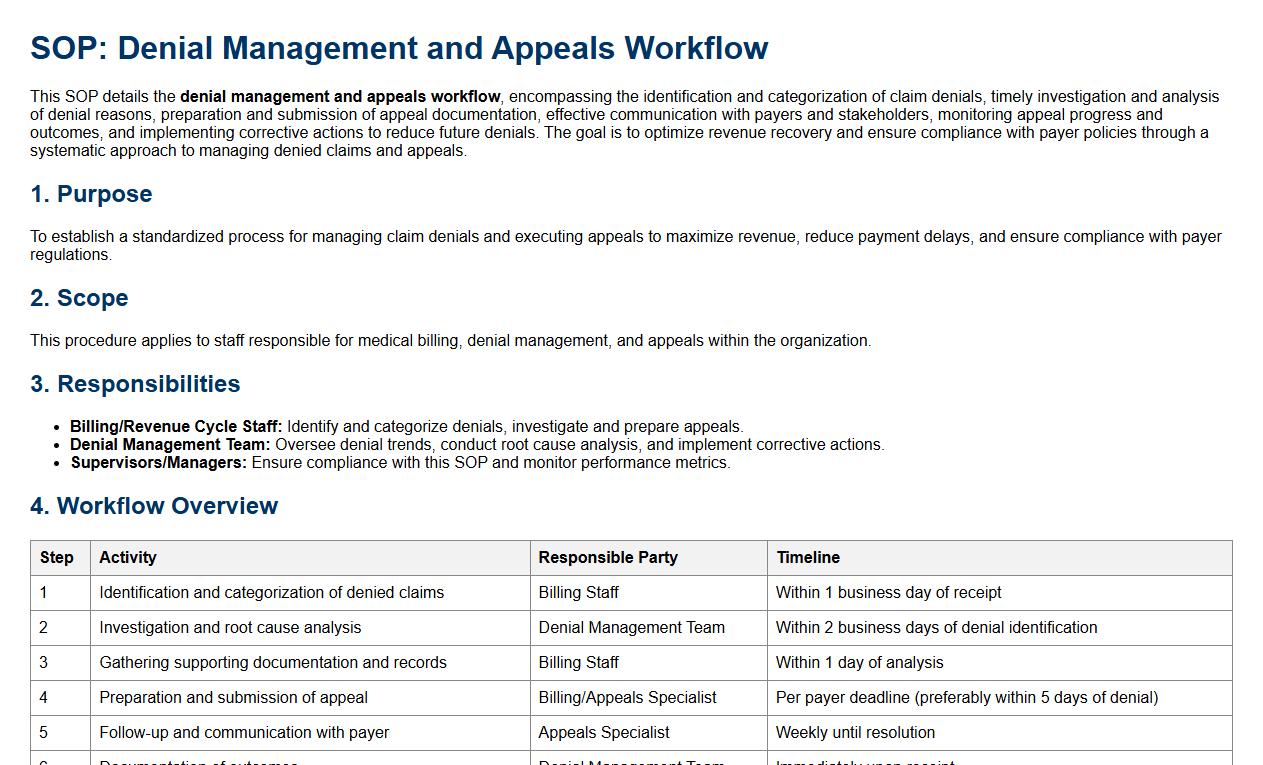
This SOP details the denial management and appeals workflow, encompassing the identification and categorization of claim denials, timely investigation and analysis of denial reasons, preparation and submission of appeal documentation, effective communication with payers and stakeholders, monitoring appeal progress and outcomes, and implementing corrective actions to reduce future denials. The goal is to optimize revenue recovery and ensure compliance with payer policies through a systematic approach to managing denied claims and appeals.
Patient billing, statements, and collections handling.
This SOP details the patient billing, statements, and collections handling process, encompassing accurate billing practices, timely generation and dispatch of patient statements, management of payment plans, insurance claim coordination, and effective collection strategies. Its objective is to ensure efficient financial operations, maintain clear communication with patients regarding their billing status, and facilitate the resolution of outstanding balances while adhering to regulatory compliance and patient confidentiality standards.
Compliance with HIPAA and data security protocols.
This SOP details the requirements for compliance with HIPAA and data security protocols, emphasizing the protection of sensitive health information, adherence to privacy regulations, implementation of secure data handling practices, employee training on confidentiality, regular security audits, breach notification procedures, and updated policies to maintain data integrity and safeguard patient information against unauthorized access or disclosures.
Monthly reporting, performance review, and audit trail documentation.
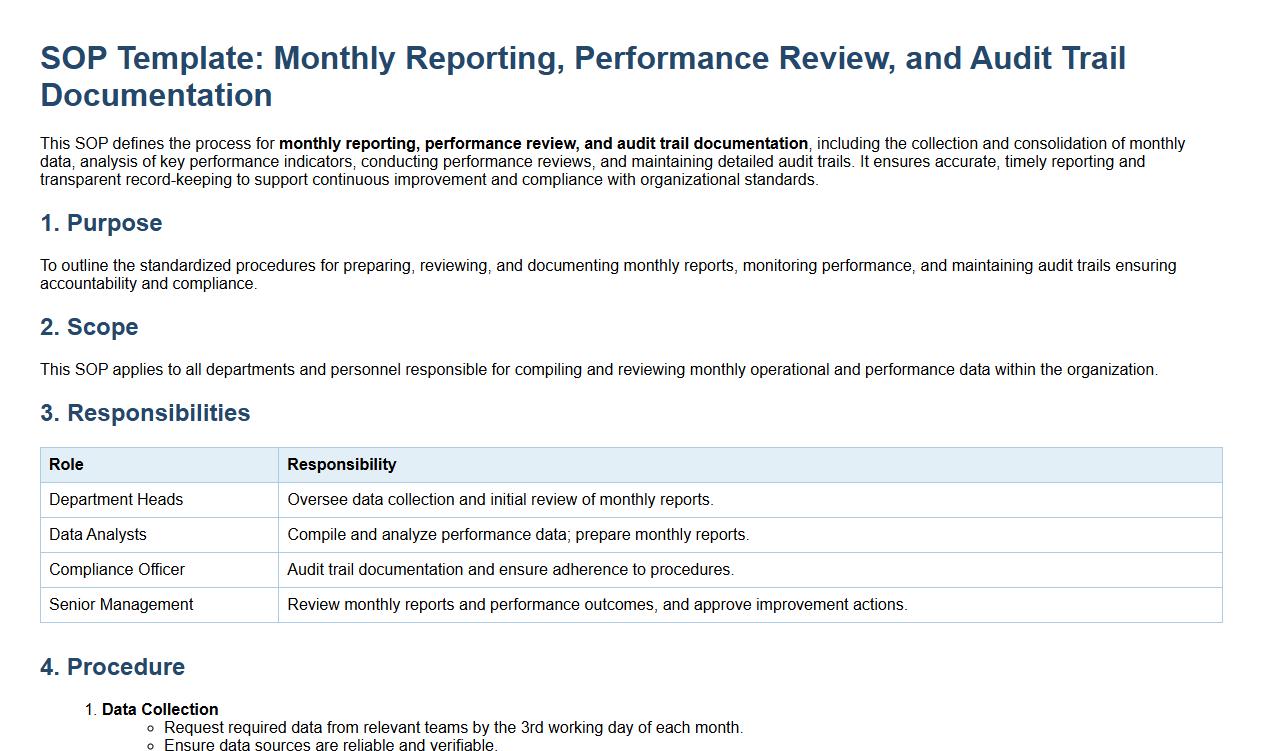
This SOP defines the process for monthly reporting, performance review, and audit trail documentation, including the collection and consolidation of monthly data, analysis of key performance indicators, conducting performance reviews, and maintaining detailed audit trails. It ensures accurate, timely reporting and transparent record-keeping to support continuous improvement and compliance with organizational standards.
Key Steps in Patient Demographic Data Entry
The SOP emphasizes accurate patient demographic data entry as the foundation for medical billing services. It mandates verification of patient details against official documents to prevent errors. Data must be entered promptly into the system to ensure seamless downstream billing processes.
Ensuring Accuracy and Timeliness in Insurance Verification
The SOP requires a thorough insurance verification process before service delivery to confirm coverage. It specifies timelines for verification to avoid delays in billing cycles. Automated tools and manual cross-checks are combined to maximize accuracy.
Standard Protocols for Claim Submission and Handling Denials
Claims must be submitted in compliance with payer requirements, as outlined in the SOP's claim submission protocols. The SOP details systematic follow-up procedures for handling claim denials to expedite resolution. Documentation of each step ensures accountability and traceability.
Compliance and Security Measures for PHI
The SOP defines strict compliance and security measures to protect Protected Health Information during billing. It includes guidelines aligned with HIPAA regulations to safeguard patient privacy. Access controls and encryption techniques are mandated for data handling.
Escalation and Reporting Procedures for Billing Discrepancies
The SOP establishes clear escalation and reporting protocols for unresolved billing discrepancies. Issues that cannot be resolved at the initial level are promptly escalated to higher management. Comprehensive reporting ensures transparency and continuous process improvement.
