A SOP template for medical billing and coding provides a structured framework to standardize billing procedures and coding accuracy within healthcare organizations. It ensures compliance with regulatory standards, reduces errors, and streamlines the claims process for faster reimbursement. This template is essential for training staff and maintaining consistency in medical billing operations.
Patient information intake and verification procedures.
This SOP details the patient information intake and verification procedures, encompassing the collection of accurate personal and medical data, verification of identity through valid documentation, confirmation of insurance and contact details, and adherence to privacy and confidentiality standards. The procedure ensures thorough and reliable patient information management to support quality healthcare delivery and comply with regulatory requirements.
Insurance eligibility and coverage verification process.
This SOP details the insurance eligibility and coverage verification process, including steps to verify patient insurance details, confirm coverage benefits, identify co-pays and deductibles, handle prior authorizations, update patient records, and communicate with insurance providers. The goal is to ensure accurate and efficient verification of insurance information to facilitate billing, reduce claim denials, and enhance patient service.
Medical coding guidelines and code assignment protocol.
This SOP details the medical coding guidelines and code assignment protocol, encompassing accurate diagnosis and procedure code selection, adherence to ICD, CPT, and HCPCS coding standards, documentation requirements, coding validation and quality control, handling of coding discrepancies and appeals, and ongoing coder training. The objective is to ensure precise code assignment for billing, reporting, and compliance purposes, thereby optimizing revenue cycle management and supporting healthcare data accuracy.
Charge capture and encounter documentation standards.
This SOP details charge capture and encounter documentation standards, outlining the procedures for accurately recording patient encounters, ensuring compliance with billing requirements, and maintaining thorough documentation for clinical and administrative purposes. It emphasizes the importance of accurate data entry, timely updates, and adherence to regulatory guidelines to optimize revenue cycle management and improve patient care delivery.
Claims creation, review, and submission workflow.
This SOP details the claims creation, review, and submission workflow, encompassing the systematic process of initiating claims, verifying accuracy and completeness through thorough review, and ensuring timely and compliant submission to relevant parties. It aims to streamline claim management, minimize errors, enhance communication between departments, and guarantee adherence to regulatory and organizational standards, ultimately facilitating efficient claims processing and resolution.
Denial management and appeals submission procedures.
This SOP details the denial management and appeals submission procedures, covering the identification and documentation of claim denials, root cause analysis, timely appeal preparation and submission, communication with payers, tracking appeal statuses, and continuous process improvement to reduce future denials. The goal is to optimize revenue recovery and ensure accurate reimbursement through effective management of denied claims and structured appeals.
Payment posting and reconciliation steps.
This SOP details the payment posting and reconciliation steps, including the accurate recording of incoming payments, verification of payment details against invoices, updating financial records, resolving discrepancies, and ensuring that all transactions are properly matched to customer accounts. The procedure aims to maintain financial accuracy, improve cash flow tracking, and ensure accountability in the payment processing workflow.
Patient billing and statement issuance protocols.
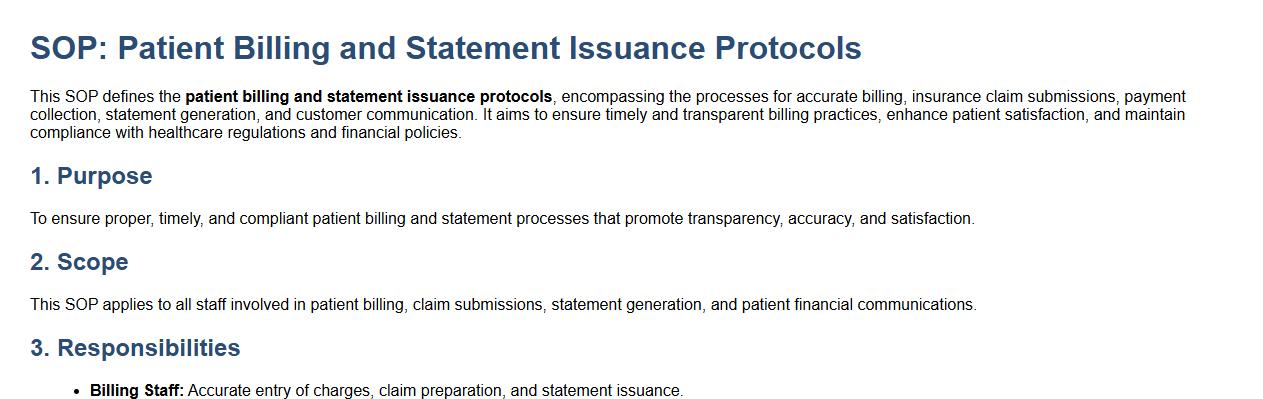
This SOP defines the patient billing and statement issuance protocols, encompassing the processes for accurate billing, insurance claim submissions, payment collection, statement generation, and customer communication. It aims to ensure timely and transparent billing practices, enhance patient satisfaction, and maintain compliance with healthcare regulations and financial policies.
Compliance checks and HIPAA privacy safeguards.
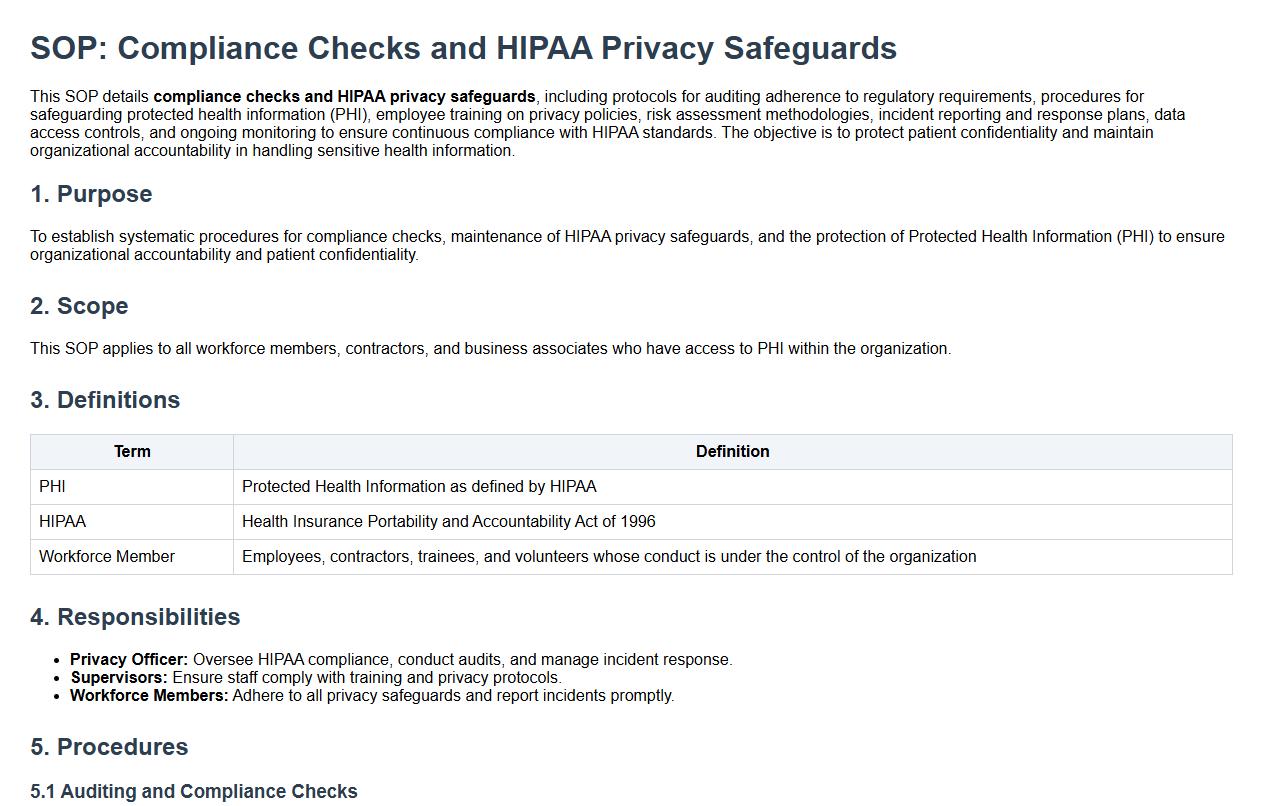
This SOP details compliance checks and HIPAA privacy safeguards, including protocols for auditing adherence to regulatory requirements, procedures for safeguarding protected health information (PHI), employee training on privacy policies, risk assessment methodologies, incident reporting and response plans, data access controls, and ongoing monitoring to ensure continuous compliance with HIPAA standards. The objective is to protect patient confidentiality and maintain organizational accountability in handling sensitive health information.
Reporting, auditing, and record retention requirements.
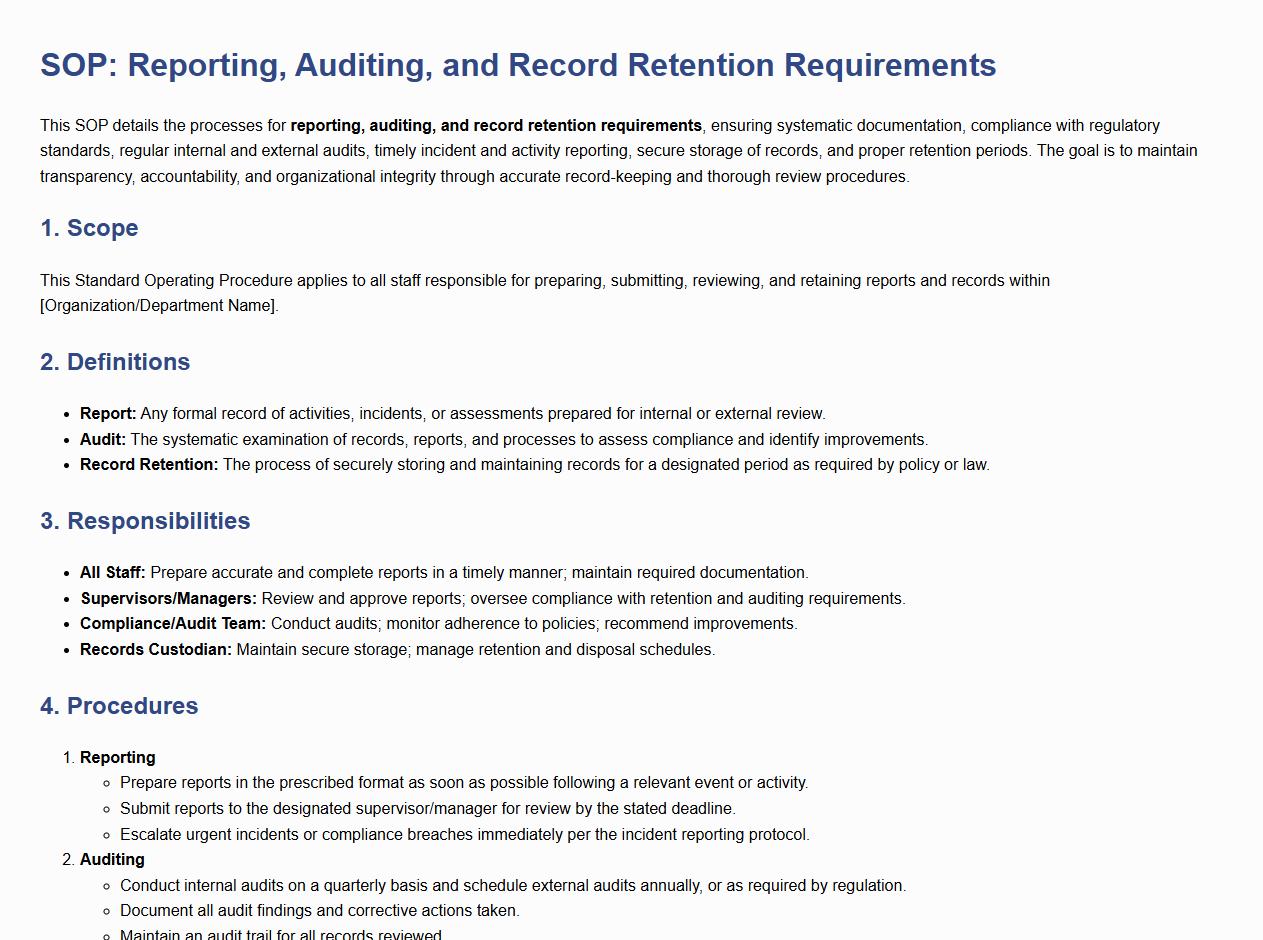
This SOP details the processes for reporting, auditing, and record retention requirements, ensuring systematic documentation, compliance with regulatory standards, regular internal and external audits, timely incident and activity reporting, secure storage of records, and proper retention periods. The goal is to maintain transparency, accountability, and organizational integrity through accurate record-keeping and thorough review procedures.
Key Steps for Accurate Patient Data Entry in Medical Billing and Coding
The SOP emphasizes the importance of comprehensive patient demographic verification to ensure data accuracy. It mandates double-checking insurance details and medical histories to reduce errors. Additionally, the process includes standardized data entry protocols to maintain consistency throughout billing.
Ensuring Compliance with HIPAA and Regulatory Requirements
The SOP incorporates strict guidelines for handling patient information in accordance with HIPAA privacy rules. It enforces secure data storage and controlled access to sensitive healthcare data. Regular employee training and audit trails are required to maintain compliance with federal regulations.
Procedures for Resolving Claim Denials and Rejections
The SOP outlines a systematic approach for identifying denial reasons, including incomplete or incorrect coding. It requires timely communication with insurers and prompt resubmission of corrected claims. Documentation of all denial resolutions is essential for tracking and improving billing practices.
Guidelines for Correct CPT, ICD-10, and HCPCS Code Selection
The SOP provides detailed instructions on using current and accurate coding manuals and software. Coders must verify clinical documentation before assigning CPT, ICD-10, and HCPCS codes. This ensures compliance with coding standards and reduces the risk of claim rejections.
Quality Assurance Measures for Billing Accuracy and Fraud Prevention
The SOP includes routine audits and cross-checks to verify the accuracy of billing data. It promotes the use of automated tools to detect anomalies indicating potential fraud or abuse. Continuous education and compliance monitoring help maintain high standards in medical billing operations.
