A SOP Template for Patient Discharge Process ensures a standardized and efficient workflow for safely releasing patients from healthcare facilities. This template outlines critical steps, including documentation, patient education, and follow-up instructions, to enhance communication between medical staff and patients. Proper use of this SOP minimizes errors and improves overall patient satisfaction during discharge.
Patient eligibility assessment and discharge readiness confirmation.
This SOP details the process for patient eligibility assessment and discharge readiness confirmation, including criteria for evaluating patient medical status, functional abilities, and psychosocial factors. It ensures comprehensive assessment protocols are followed to determine eligibility for discharge, coordinate multidisciplinary team input, plan for post-discharge care, and confirm patient and family understanding of discharge instructions. The goal is to facilitate safe, timely, and appropriate transitions from healthcare facilities to home or other care settings.
Physician approval and completion of discharge orders.
This SOP details the process for physician approval and completion of discharge orders, ensuring timely and accurate authorization by the attending physician prior to patient discharge. It covers verification of patient readiness, review of discharge instructions, medication reconciliation, and coordination with multidisciplinary teams to facilitate safe and effective patient transition from hospital to home or other care settings.
Preparation and review of patient discharge summary.
This SOP details the preparation and review of patient discharge summary, outlining the process of compiling comprehensive and accurate patient information, including diagnosis, treatment provided, medications prescribed, follow-up instructions, and any necessary referrals. It emphasizes the importance of timely preparation, thorough review by healthcare professionals, and clear communication to ensure continuity of care and patient safety upon discharge.
Medication reconciliation and prescription arrangement.
This SOP details the process of medication reconciliation and prescription arrangement, emphasizing accurate verification of patients' medication lists, identification and resolution of discrepancies, coordination with healthcare providers for prescription updates, and ensuring safe and effective medication management. The goal is to enhance patient safety by preventing medication errors and ensuring clear communication across care transitions.
Patient and caregiver discharge education and counseling.
This SOP defines the process of patient and caregiver discharge education and counseling, ensuring that patients and their caregivers receive comprehensive instructions regarding post-discharge care, medication management, follow-up appointments, lifestyle modifications, and warning signs for complications. The goal is to improve patient outcomes, enhance understanding of discharge plans, and support a smooth transition from hospital to home care.
Coordination of follow-up appointments and referrals.
This SOP details the coordination of follow-up appointments and referrals, outlining the procedures for scheduling patient follow-ups, managing referral communications, ensuring timely information exchange between healthcare providers, and tracking patient compliance. The goal is to enhance continuity of care, improve patient outcomes, and streamline administrative processes by effective coordination and documentation of all follow-up and referral activities.
Arrangement of transportation and post-discharge support services.
This SOP details the arrangement of transportation and post-discharge support services, encompassing the coordination of patient transport logistics, ensuring timely and safe transfers, organizing follow-up care, providing necessary support for recovery at home, and facilitating communication between healthcare providers and patients. The objective is to enhance patient experience and continuity of care by delivering efficient transportation solutions and comprehensive post-discharge assistance.
Final nursing assessment and vital sign documentation.
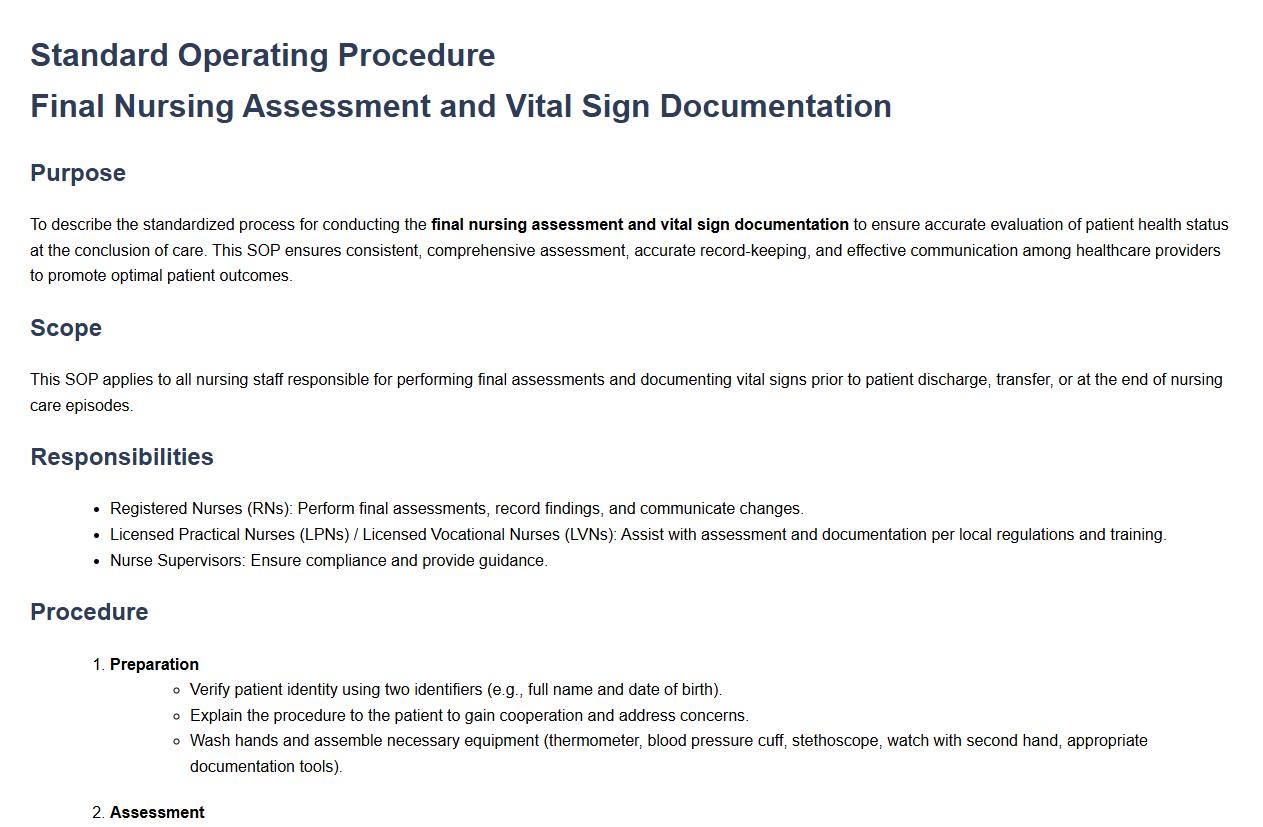
This SOP details the process for conducting the final nursing assessment and vital sign documentation, ensuring accurate evaluation of patient health status at the conclusion of care. It covers the systematic review of patient condition, measurement of vital signs including temperature, pulse, respiration, and blood pressure, and the precise recording of all findings in the patient's medical record. The purpose is to guarantee comprehensive patient monitoring, effective communication among healthcare providers, and the promotion of optimal patient outcomes through consistent and thorough documentation practices.
Collection and return of hospital property and patient belongings.
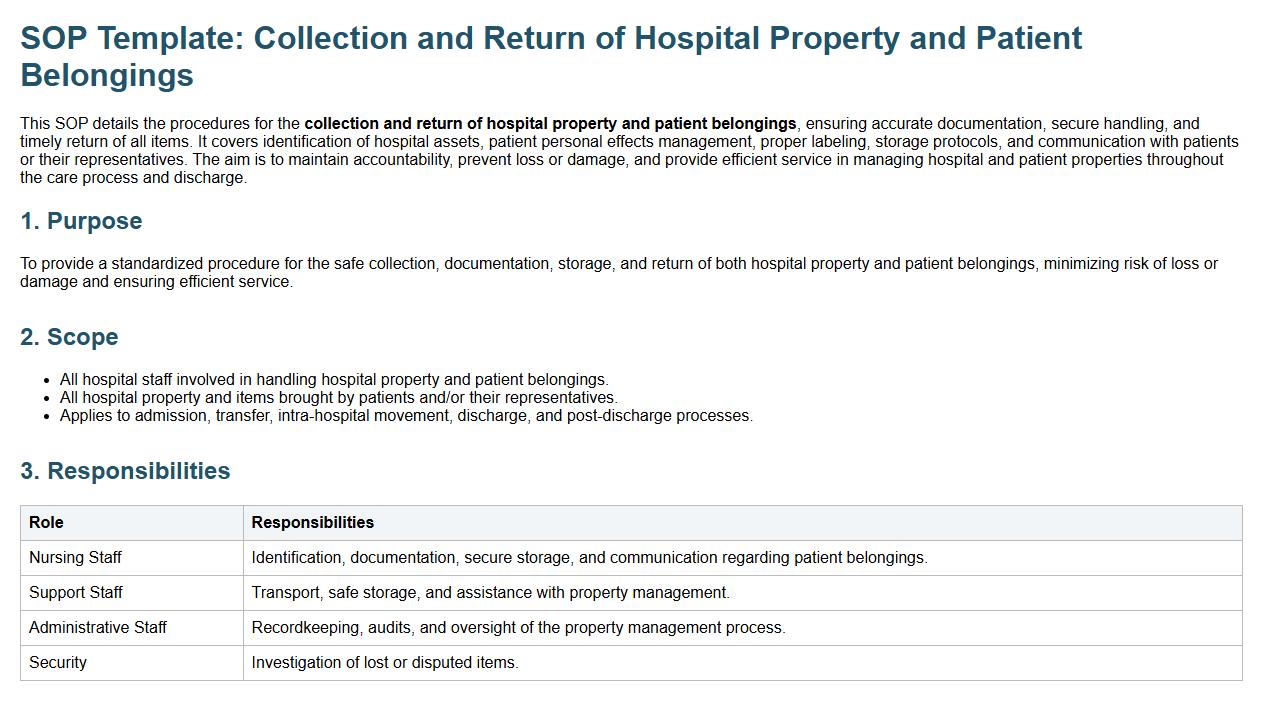
This SOP details the procedures for the collection and return of hospital property and patient belongings, ensuring accurate documentation, secure handling, and timely return of all items. It covers identification of hospital assets, patient personal effects management, proper labeling, storage protocols, and communication with patients or their representatives. The aim is to maintain accountability, prevent loss or damage, and provide efficient service in managing hospital and patient properties throughout the care process and discharge.
Completion of discharge documentation and reporting.
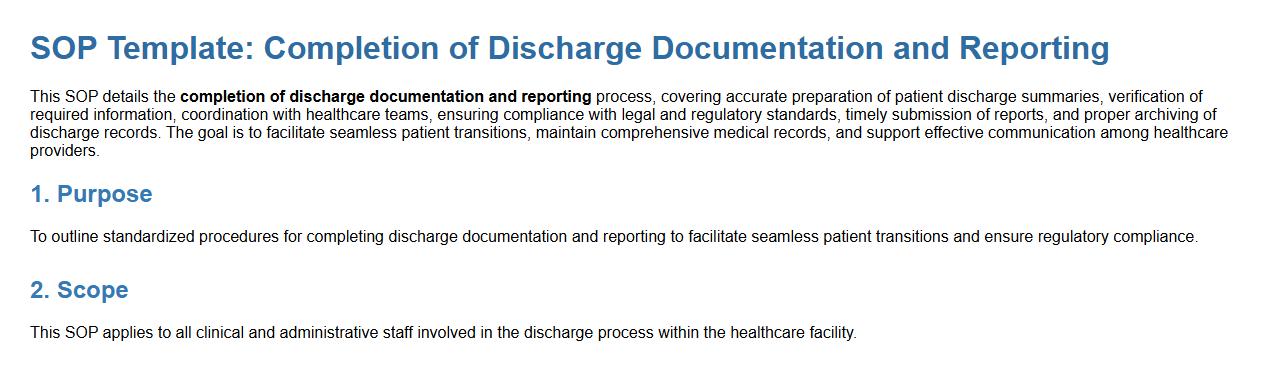
This SOP details the completion of discharge documentation and reporting process, covering accurate preparation of patient discharge summaries, verification of required information, coordination with healthcare teams, ensuring compliance with legal and regulatory standards, timely submission of reports, and proper archiving of discharge records. The goal is to facilitate seamless patient transitions, maintain comprehensive medical records, and support effective communication among healthcare providers.
What essential patient information must be verified and documented before initiating the discharge process?
Before initiating the discharge process, it is crucial to verify and document the patient's identity, contact details, and insurance information. Confirming the patient's clinical status, including recent lab results and treatment summaries, ensures safe discharge. Additionally, documenting any allergies and current medications is essential to prevent errors post-discharge.
Which key staff members are required to participate in the patient discharge workflow as per SOP?
The discharge workflow mandates participation from interdisciplinary team members such as physicians, nurses, and case managers. Pharmacists play a critical role in reviewing and reconciling medications before discharge. Social workers and discharge planners coordinate additional support services and patient education to ensure comprehensive care.
What standard instructions and educational materials must be provided to patients during discharge?
Patients must receive clear written and verbal instructions covering medication regimens, activity restrictions, and diet modifications. Educational materials tailored to the patient's diagnosis and care plan facilitate understanding and compliance. It is also essential to provide information on symptom monitoring and when to seek medical attention.
How should medication reconciliation be handled and documented according to the SOP?
Medication reconciliation requires a thorough review of all prescribed, over-the-counter, and complementary medicines to ensure accuracy. This process must be witnessed and documented by both the pharmacist and the attending physician in the patient's medical record. Proper documentation prevents adverse drug events and supports continuity of care post-discharge.
What are the mandatory steps for follow-up coordination and communication with outpatient care providers?
Follow-up coordination includes scheduling outpatient appointments and ensuring transfer of relevant medical records. Communication with primary care providers and specialists must be documented to ensure continuity of care. Additionally, confirmation of patient understanding and compliance with follow-up plans is essential for successful recovery.
