
A SOP Template for Nursing Shift Handover ensures a standardized process for transferring patient care responsibilities between nursing staff. It enhances communication, reduces errors, and maintains continuity of care by providing clear guidelines and checklists. Using this template improves efficiency and patient safety during shift changes.
Patient Identification and Verification procedure.
This SOP details the patient identification and verification procedure, emphasizing accurate patient recognition methods to prevent errors. It covers the use of multiple identifiers such as name, date of birth, and medical record number, verification processes before administering treatments or procedures, and communication protocols among healthcare providers. The objective is to enhance patient safety, reduce the risk of misidentification, and ensure proper delivery of care throughout the healthcare system.
Shift Start-Time and Attendance Recording.
This SOP details the procedures for shift start-time and attendance recording, including accurate employee clock-in methods, verification of shift schedules, handling of late arrivals and early departures, and maintenance of attendance logs. The objective is to ensure precise tracking of employee attendance, enhance shift management efficiency, and support payroll accuracy.
Medication Administration Handover and Reconciliation.
This SOP details the medication administration handover and reconciliation process, ensuring accurate communication and documentation during patient care transitions. It covers standardized procedures for transferring medication information between healthcare providers, verifying medication lists to prevent errors, and maintaining updated records to promote patient safety and continuity of care.
Vital Signs and Observation Documentation Transfer.
This SOP describes the process for vital signs and observation documentation transfer, detailing the accurate recording, timely updating, and secure communication of patient vital signs and clinical observations between healthcare providers. It ensures continuity of care, minimizes errors, and supports effective clinical decision-making by standardizing the transfer of critical patient information during shift changes, patient transfers, or handovers.
Current and Pending Doctor’s Orders Review.
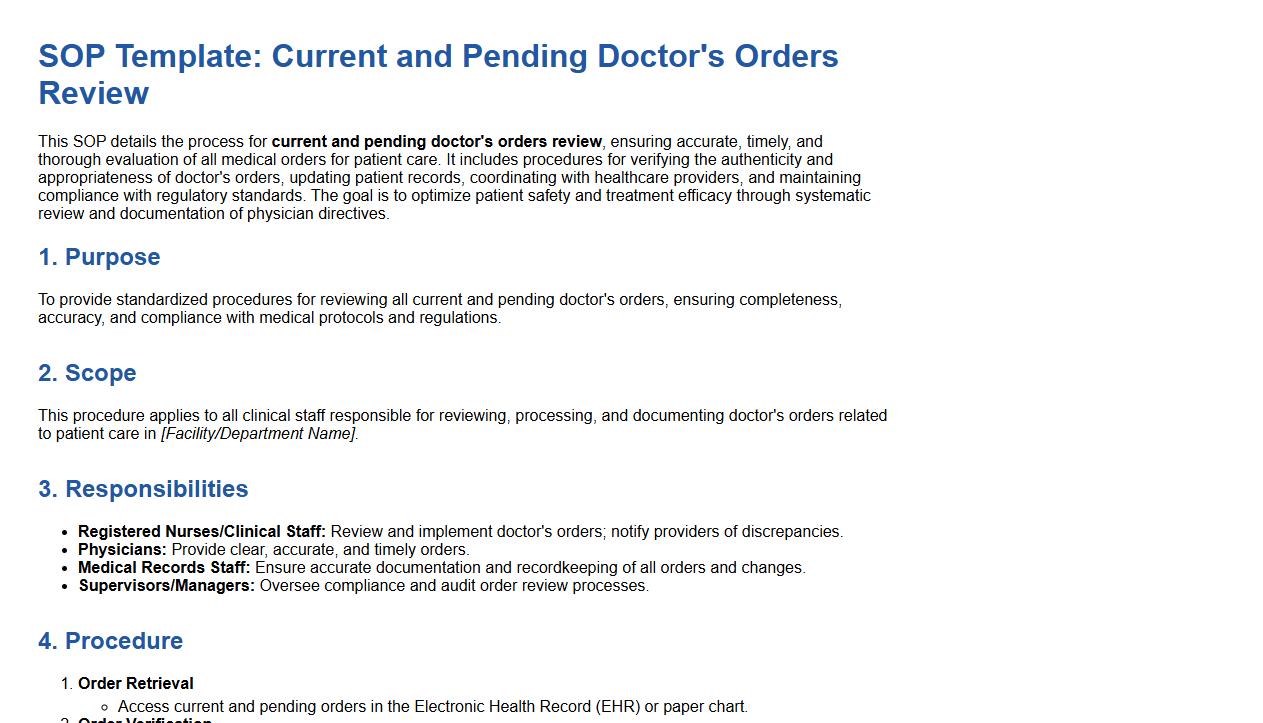
This SOP details the process for current and pending doctor's orders review, ensuring accurate, timely, and thorough evaluation of all medical orders for patient care. It includes procedures for verifying the authenticity and appropriateness of doctor's orders, updating patient records, coordinating with healthcare providers, and maintaining compliance with regulatory standards. The goal is to optimize patient safety and treatment efficacy through systematic review and documentation of physician directives.
Outstanding Nursing Assessments and Interventions Checklist.
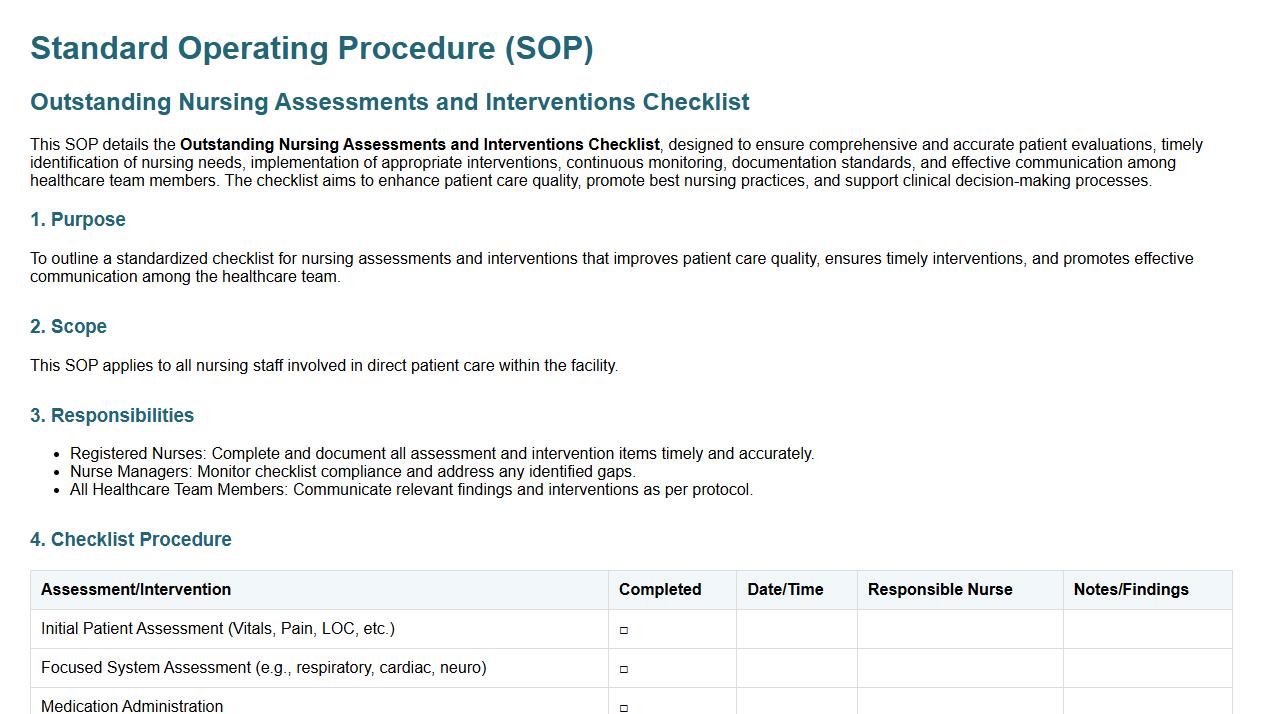
This SOP details the Outstanding Nursing Assessments and Interventions Checklist, designed to ensure comprehensive and accurate patient evaluations, timely identification of nursing needs, implementation of appropriate interventions, continuous monitoring, documentation standards, and effective communication among healthcare team members. The checklist aims to enhance patient care quality, promote best nursing practices, and support clinical decision-making processes.
Incident and Unusual Event Reporting Process.
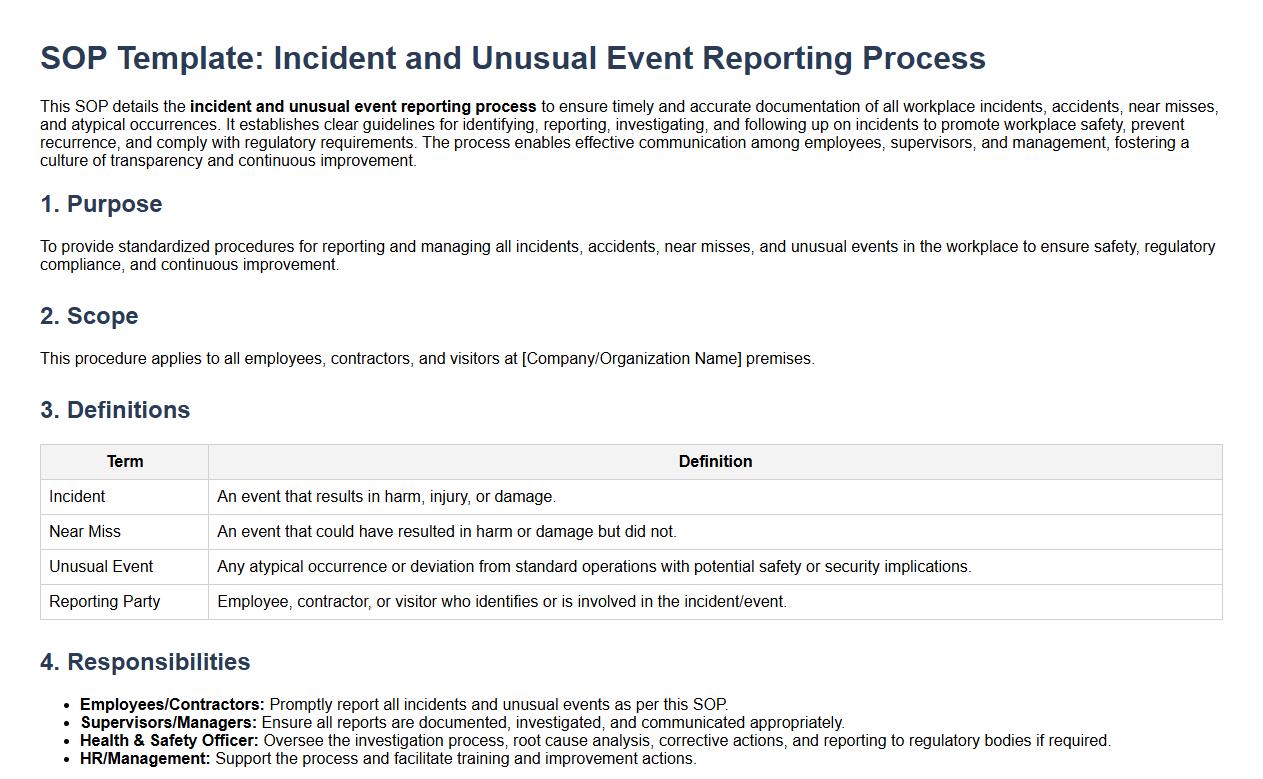
This SOP details the incident and unusual event reporting process to ensure timely and accurate documentation of all workplace incidents, accidents, near misses, and atypical occurrences. It establishes clear guidelines for identifying, reporting, investigating, and following up on incidents to promote workplace safety, prevent recurrence, and comply with regulatory requirements. The process enables effective communication among employees, supervisors, and management, fostering a culture of transparency and continuous improvement.
Infection Control and Isolation Status Updates.
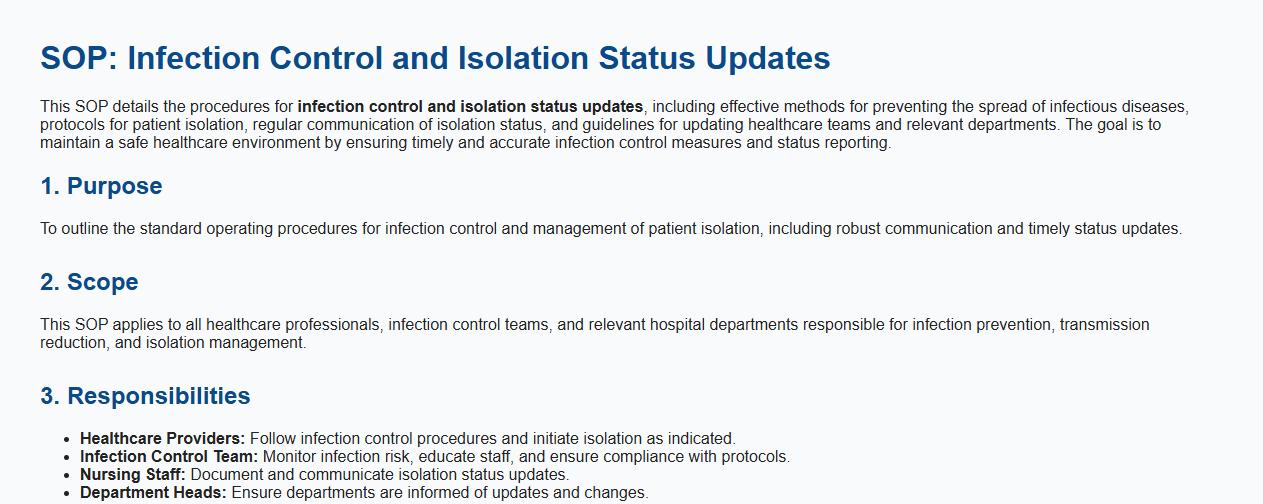
This SOP details the procedures for infection control and isolation status updates, including effective methods for preventing the spread of infectious diseases, protocols for patient isolation, regular communication of isolation status, and guidelines for updating healthcare teams and relevant departments. The goal is to maintain a safe healthcare environment by ensuring timely and accurate infection control measures and status reporting.
Communication of Special Patient Needs and Risks.
This SOP details the processes for the communication of special patient needs and risks, ensuring that all healthcare providers are informed about unique patient requirements, potential hazards, and risk factors. It covers methods for accurate documentation, timely information sharing among medical staff, patient and family communication protocols, confidentiality considerations, and strategies to mitigate risks associated with patient care. The goal is to enhance patient safety and improve care outcomes through effective and clear communication.
Documentation of Handover Completion and Nurse Signature.
This SOP details the documentation of handover completion and nurse signature process to ensure accurate and complete transfer of patient care information between nursing shifts. It covers the required information to be recorded, the timing of documentation, verification of handover accuracy, and the formal nurse signature to confirm accountability and continuity of care. Proper execution of this procedure enhances communication, reduces errors, and supports patient safety in healthcare settings.
Essential Patient Details Required During a Nursing Shift Handover as per the SOP
The SOP mandates the inclusion of patient identification details such as name, age, and medical record number during handover. Vital signs, current medications, and recent changes in patient condition are critical to communicate clearly. Additionally, any ongoing treatments and care plans must be accurately shared to ensure continuity of care.
Standardized Communication Method Mandated in the Handover Process
The SOP requires the use of the SBAR (Situation, Background, Assessment, Recommendation) method to structure handover communication. This ensures clarity, completeness, and uniformity in information transfer between nursing shifts. SBAR promotes effective teamwork and reduces the risk of errors during shift changeovers.
Documentation of Critical Incidents During Handover
The SOP emphasizes documenting any critical incidents that occurred during the shift in the official nursing notes and incident reports. This documentation is essential for accountability and facilitates prompt follow-up actions. Clear records allow the incoming nurse to be fully aware of patient safety concerns.
Steps to Verify Understanding and Clarify Doubts During Shift Change
Nurses are required to actively engage in feedback and question sessions during handover to verify understanding. The SOP encourages repeating important information and asking clarifying questions to avoid misunderstandings. Ensuring mutual comprehension helps maintain patient safety and care quality.
Guidelines for Handling Incomplete or Missing Information During Handover
The SOP advises nurses to immediately flag any incomplete or missing patient information to the outgoing nurse or supervisor. Nurses should document these gaps and initiate follow-up actions to obtain the necessary data. This proactive approach helps prevent potential risks associated with incomplete handover information.
