
A SOP Template for Hospital Billing Process ensures standardized procedures for accurate and efficient patient billing. It outlines step-by-step guidelines for verifying insurance details, generating invoices, and processing payments. This template helps reduce errors, streamline workflow, and maintain compliance with healthcare regulations.
Patient registration and verification of personal and insurance details.
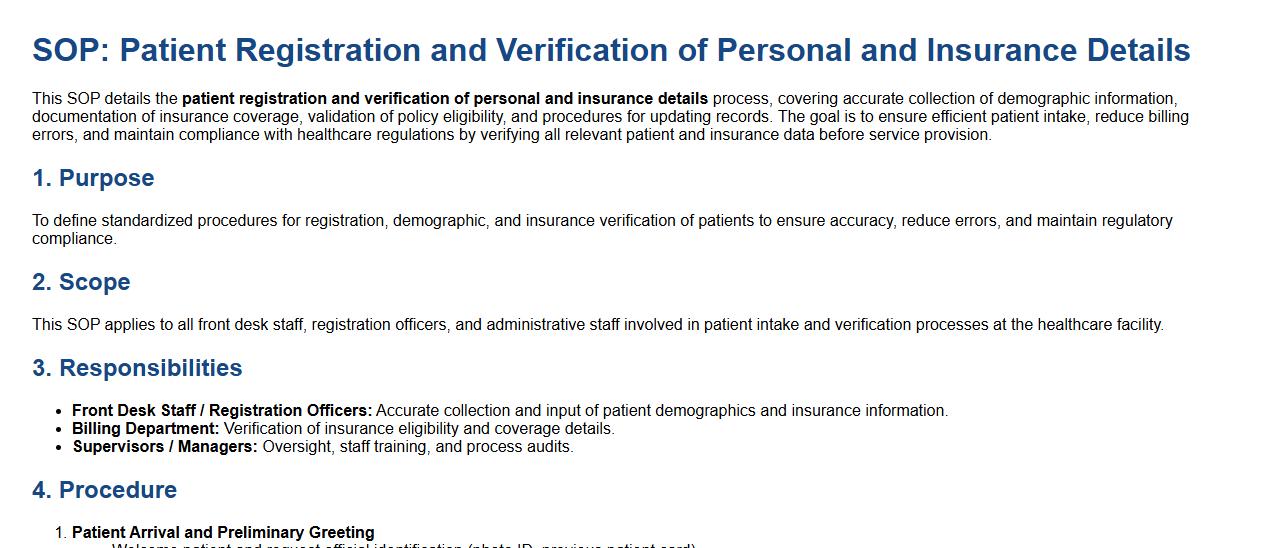
This SOP details the patient registration and verification of personal and insurance details process, covering accurate collection of demographic information, documentation of insurance coverage, validation of policy eligibility, and procedures for updating records. The goal is to ensure efficient patient intake, reduce billing errors, and maintain compliance with healthcare regulations by verifying all relevant patient and insurance data before service provision.
Pre-admission estimation and cost approval process.
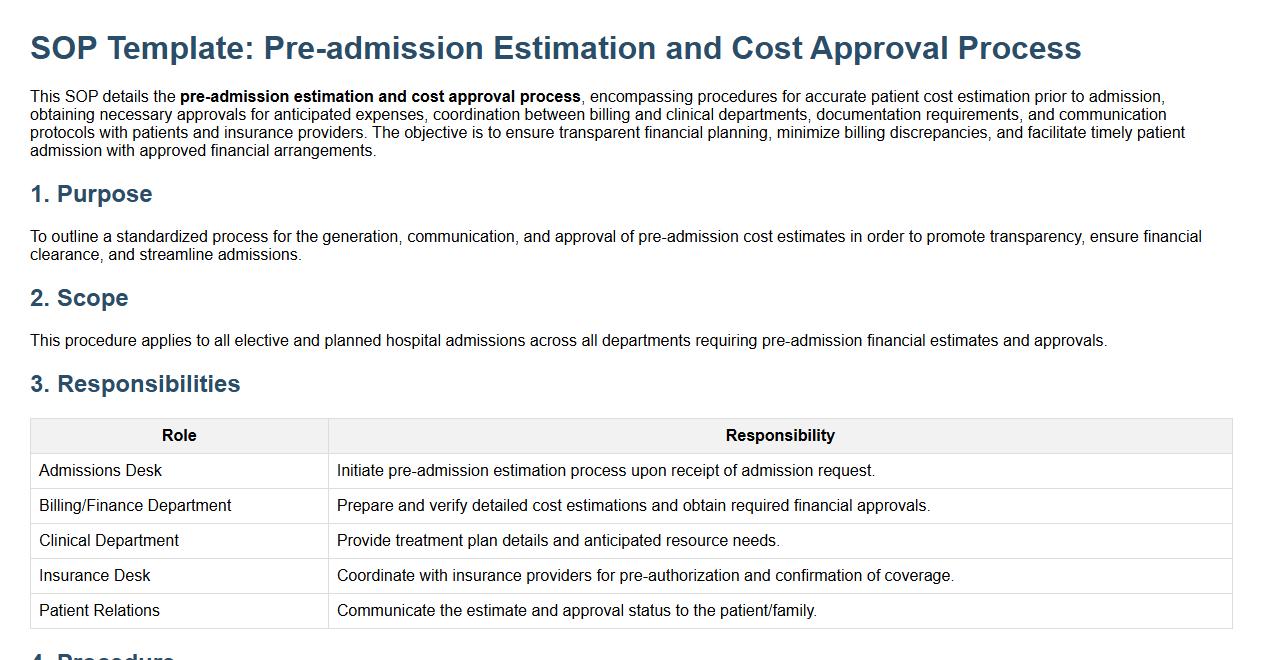
This SOP details the pre-admission estimation and cost approval process, encompassing procedures for accurate patient cost estimation prior to admission, obtaining necessary approvals for anticipated expenses, coordination between billing and clinical departments, documentation requirements, and communication protocols with patients and insurance providers. The objective is to ensure transparent financial planning, minimize billing discrepancies, and facilitate timely patient admission with approved financial arrangements.
Eligibility check and insurance coverage verification.
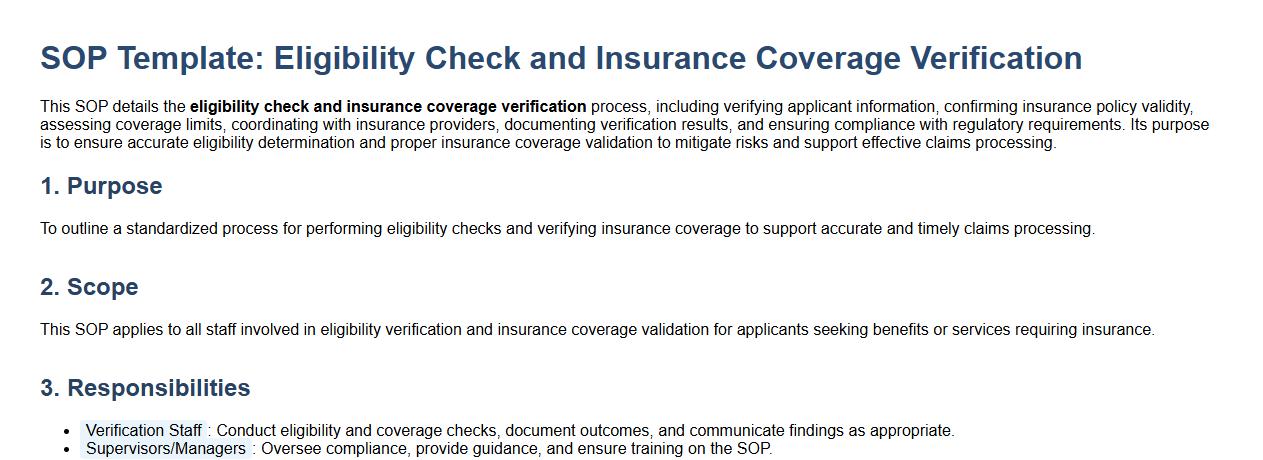
This SOP details the eligibility check and insurance coverage verification process, including verifying applicant information, confirming insurance policy validity, assessing coverage limits, coordinating with insurance providers, documenting verification results, and ensuring compliance with regulatory requirements. Its purpose is to ensure accurate eligibility determination and proper insurance coverage validation to mitigate risks and support effective claims processing.
Pre-authorization request submission and tracking.
This SOP details the process for pre-authorization request submission and tracking, encompassing the steps for preparing and submitting requests, required documentation, approval workflows, communication protocols, and tracking mechanisms. The objective is to ensure timely and accurate authorization for actions or expenditures, enhancing accountability and operational efficiency.
Accurate charging for services rendered and coding of procedures.
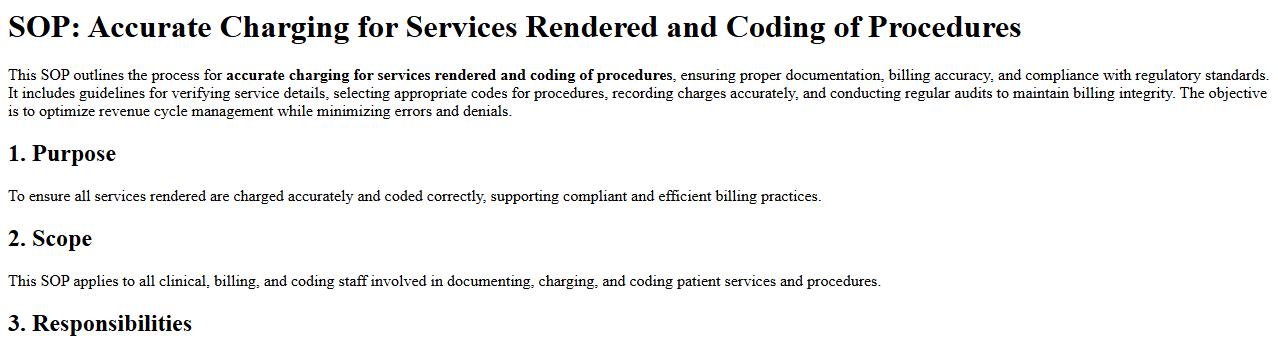
This SOP outlines the process for accurate charging for services rendered and coding of procedures, ensuring proper documentation, billing accuracy, and compliance with regulatory standards. It includes guidelines for verifying service details, selecting appropriate codes for procedures, recording charges accurately, and conducting regular audits to maintain billing integrity. The objective is to optimize revenue cycle management while minimizing errors and denials.
Medical records documentation and timely submission to billing.
This SOP details the process for medical records documentation and timely submission to billing, emphasizing accurate and complete patient record keeping, compliance with healthcare regulations, efficient data entry, verification of coding and billing information, and prompt transmission of records to the billing department. The goal is to enhance revenue cycle management, reduce claim denials, and ensure a seamless flow of information between clinical and administrative teams.
Preparation and generation of patient bills and invoices.
This SOP details the preparation and generation of patient bills and invoices, covering the processes of accurately recording patient services, calculating charges based on treatments and procedures, verifying patient insurance and payment information, and issuing clear and itemized invoices. The purpose is to ensure timely and precise billing to facilitate effective financial management, enhance patient satisfaction, and maintain compliance with healthcare regulations and billing standards.
Claims submission to insurance providers and follow-up.
This SOP details the process for claims submission to insurance providers and follow-up, covering the accurate preparation and timely submission of insurance claims, verification of required documentation, communication protocols with insurance companies, tracking claim status, resolving discrepancies or denials, and ensuring prompt reimbursement. The objective is to streamline claims management, reduce errors, and improve the efficiency of insurance claim processing to support financial stability and compliance.
Handling patient queries, billing disputes, and corrections.
This SOP details the process for handling patient queries, billing disputes, and corrections, including steps for receiving and logging inquiries, verifying patient information, investigating billing discrepancies, communicating resolutions effectively, processing necessary billing adjustments, and maintaining accurate records. The aim is to ensure prompt, transparent, and accurate responses to patient concerns, promoting improved patient satisfaction and financial accountability.
Collection, payment posting, and reconciliation of outstanding dues.
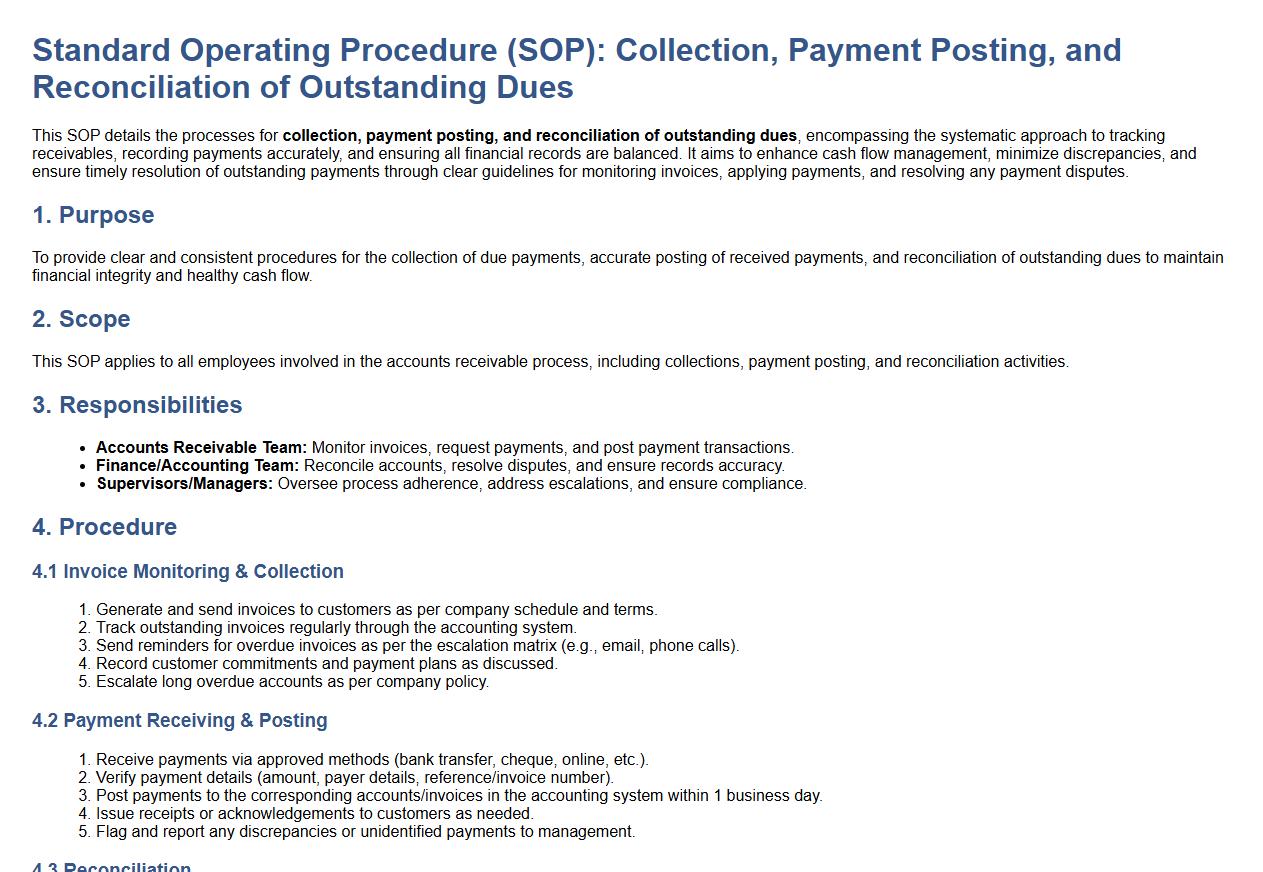
This SOP details the processes for collection, payment posting, and reconciliation of outstanding dues, encompassing the systematic approach to tracking receivables, recording payments accurately, and ensuring all financial records are balanced. It aims to enhance cash flow management, minimize discrepancies, and ensure timely resolution of outstanding payments through clear guidelines for monitoring invoices, applying payments, and resolving any payment disputes.
Key Steps for Initiating Hospital Billing Process
The SOP begins with the collection of accurate patient data to ensure billing precision. Next, it requires verification of service codes and billing rates for each treatment provided. The final step involves entering all billing information into the hospital's billing system for further processing.
Departments Responsible for Verifying Patient Billing Information
The medical records department ensures the accuracy of patient treatment details. The billing department cross-checks all financial data and insurance claims. Additionally, the admissions department confirms patient demographics and insurance eligibility before billing.
Documentation Required for Processing Inpatient versus Outpatient Bills
For inpatients, the SOP mandates detailed admission records, medical charts, and discharge summaries. Outpatient billing requires service slips, consultation notes, and procedure codes. Both processes require insurance authorization documents for claim submission.
Handling Discrepancies or Disputes in Billing
The SOP instructs staff to immediately document any billing discrepancies found during verification. Staff must engage with patients or insurance representatives to clarify and resolve issues promptly. All disputes are tracked and reviewed by the billing supervisor for final resolution.
Prescribed Timelines for Bill Generation, Review, and Patient Notification
Bills must be generated within 48 hours after patient discharge or outpatient service. The review process should be completed within 24 hours post-generation to ensure accuracy. Patients are notified via email or phone call within 72 hours after the bill is finalized.
