
A SOP Template for Post-Operative Care provides a clear, step-by-step guide to ensure consistent and effective patient management after surgery. It outlines essential protocols such as monitoring vital signs, pain management, wound care, and infection prevention. This template helps healthcare professionals maintain high standards of care and improve patient recovery outcomes.
Patient monitoring protocols.
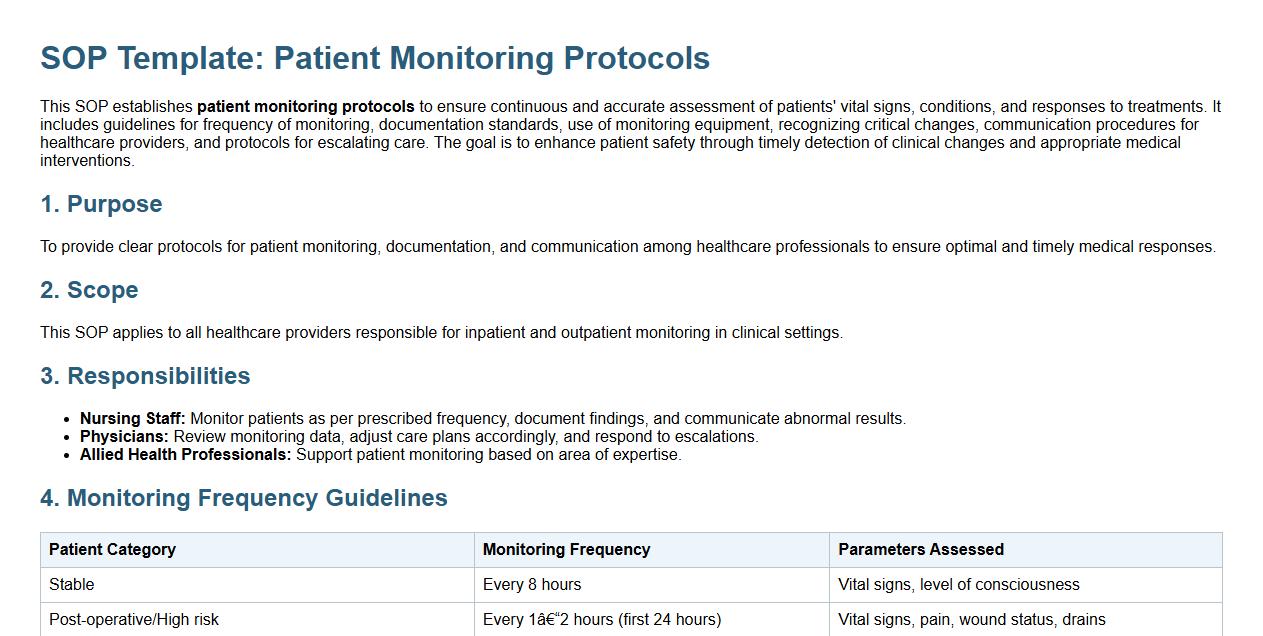
This SOP establishes patient monitoring protocols to ensure continuous and accurate assessment of patients' vital signs, conditions, and responses to treatments. It includes guidelines for frequency of monitoring, documentation standards, use of monitoring equipment, recognizing critical changes, communication procedures for healthcare providers, and protocols for escalating care. The goal is to enhance patient safety through timely detection of clinical changes and appropriate medical interventions.
Vital signs assessment schedule.
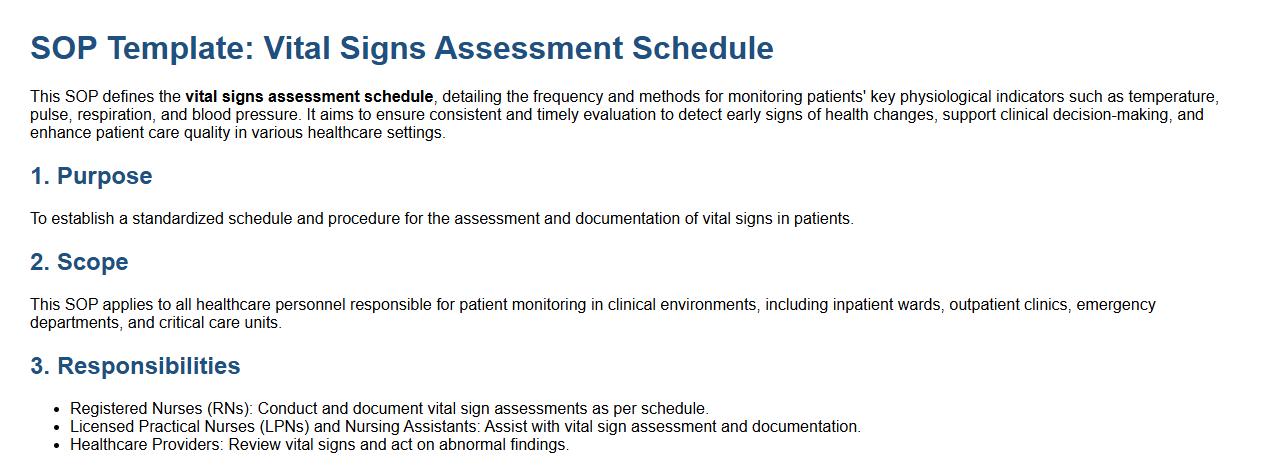
This SOP defines the vital signs assessment schedule, detailing the frequency and methods for monitoring patients' key physiological indicators such as temperature, pulse, respiration, and blood pressure. It aims to ensure consistent and timely evaluation to detect early signs of health changes, support clinical decision-making, and enhance patient care quality in various healthcare settings.
Pain management and medication administration.
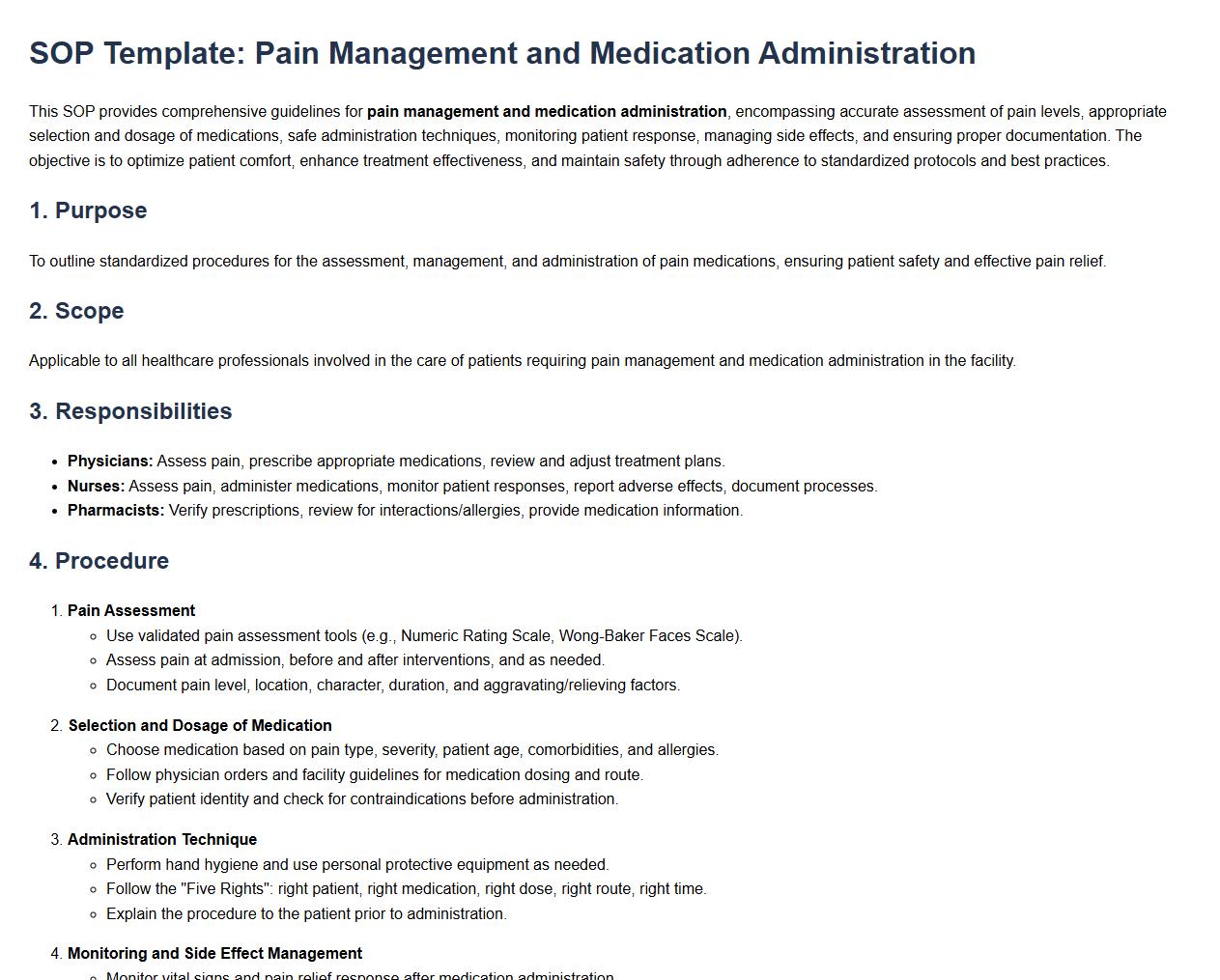
This SOP provides comprehensive guidelines for pain management and medication administration, encompassing accurate assessment of pain levels, appropriate selection and dosage of medications, safe administration techniques, monitoring patient response, managing side effects, and ensuring proper documentation. The objective is to optimize patient comfort, enhance treatment effectiveness, and maintain safety through adherence to standardized protocols and best practices.
Wound care and dressing change procedures.
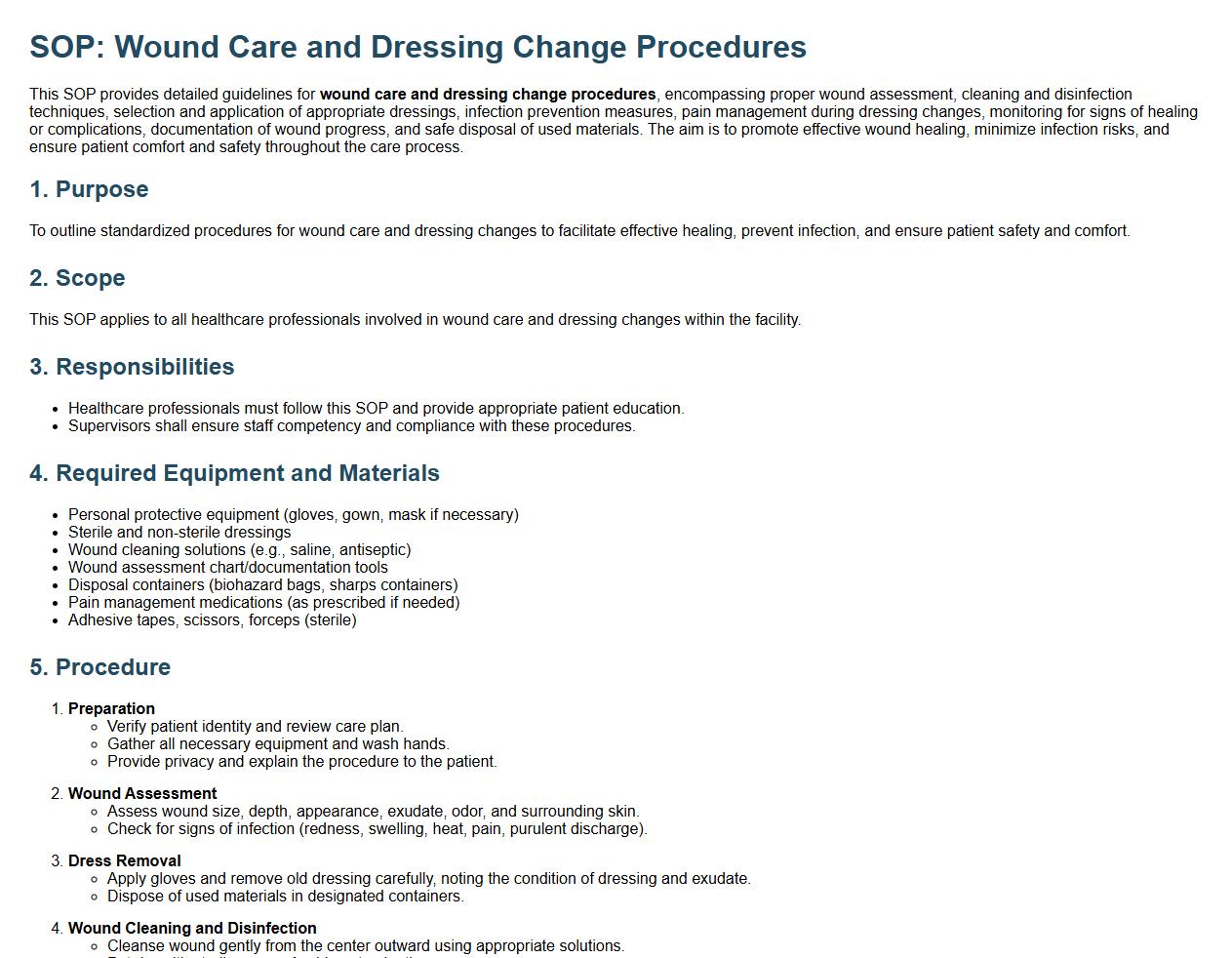
This SOP provides detailed guidelines for wound care and dressing change procedures, encompassing proper wound assessment, cleaning and disinfection techniques, selection and application of appropriate dressings, infection prevention measures, pain management during dressing changes, monitoring for signs of healing or complications, documentation of wound progress, and safe disposal of used materials. The aim is to promote effective wound healing, minimize infection risks, and ensure patient comfort and safety throughout the care process.
Infection prevention and hand hygiene practices.
This SOP details infection prevention and hand hygiene practices, including proper handwashing techniques, use of hand sanitizers, guidelines for personal protective equipment, cleaning and disinfecting protocols, and strategies to minimize the spread of infectious agents in healthcare and community settings. The objective is to reduce the risk of infection transmission and promote overall health and safety through consistent and effective hygiene practices.
Mobility and physical therapy guidelines.
This SOP details mobility and physical therapy guidelines, covering patient assessment, personalized therapy plans, proper exercise techniques, use of assistive devices, safety protocols during sessions, progress monitoring, and documentation standards. The aim is to enhance patient mobility, reduce pain, prevent injury, and promote overall physical rehabilitation through structured and evidence-based therapeutic approaches.
Nutrition and hydration management.
This SOP details nutrition and hydration management to ensure proper dietary intake and fluid balance. It covers guidelines for assessing nutritional needs, planning balanced meals, monitoring hydration status, managing special dietary requirements, and promoting healthy eating habits. The goal is to support optimal health, enhance recovery, and maintain well-being through effective nutrition and hydration practices.
Patient education and discharge planning.
This SOP details the process of patient education and discharge planning, focusing on effective communication, individualized patient teaching, medication instructions, follow-up care coordination, and ensuring patient understanding for a safe transition from hospital to home or another care setting. The goal is to enhance patient outcomes, reduce readmissions, and promote self-care through comprehensive education and organized discharge procedures.
Handling emergency or complications post-surgery.
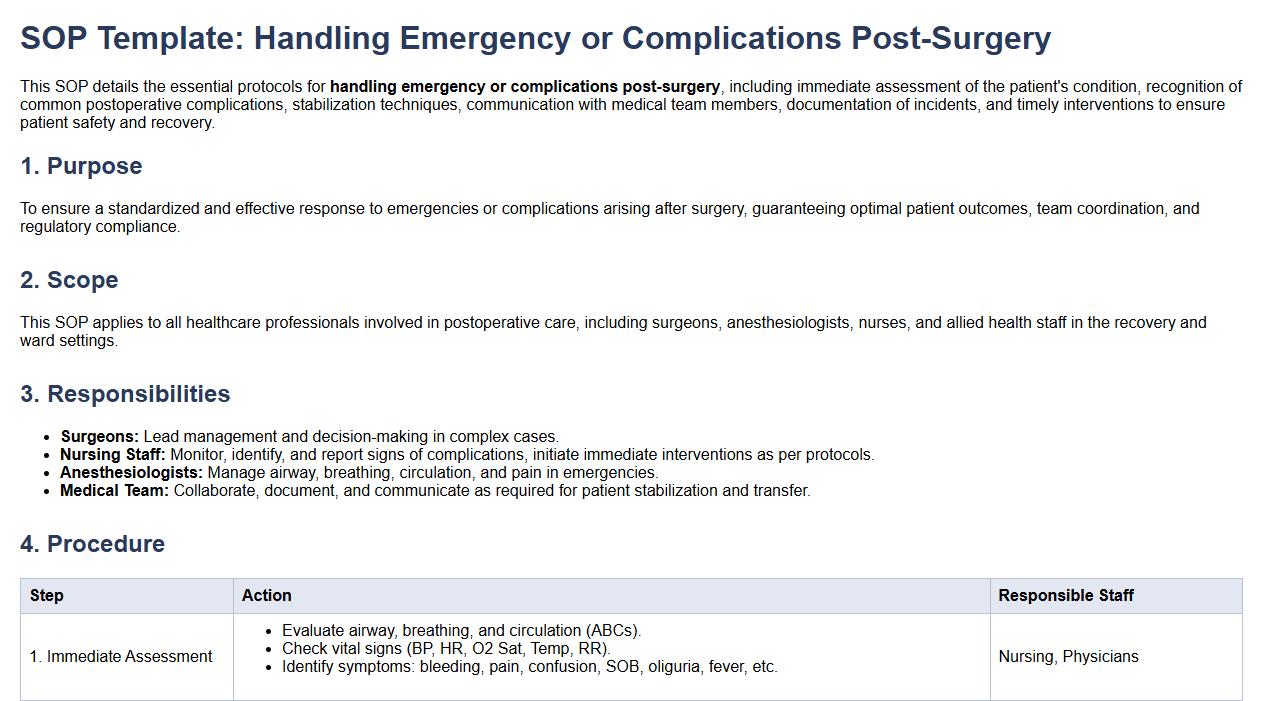
This SOP details the essential protocols for handling emergency or complications post-surgery, including immediate assessment of the patient's condition, recognition of common postoperative complications, stabilization techniques, communication with medical team members, documentation of incidents, and timely interventions to ensure patient safety and recovery.
Documentation and reporting requirements.
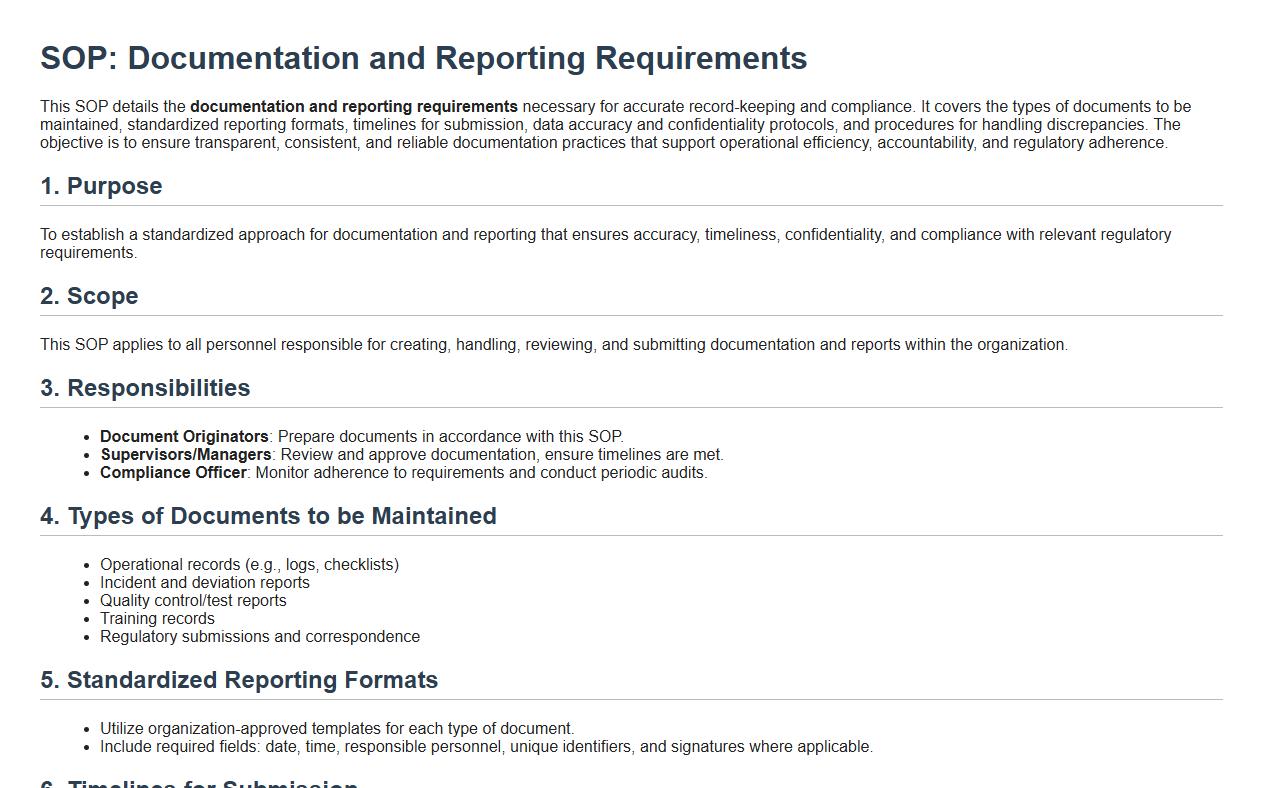
This SOP details the documentation and reporting requirements necessary for accurate record-keeping and compliance. It covers the types of documents to be maintained, standardized reporting formats, timelines for submission, data accuracy and confidentiality protocols, and procedures for handling discrepancies. The objective is to ensure transparent, consistent, and reliable documentation practices that support operational efficiency, accountability, and regulatory adherence.
What is the primary purpose of a Standard Operating Procedure (SOP) for post-operative care?
The primary purpose of a Standard Operating Procedure (SOP) for post-operative care is to ensure consistent, safe, and effective management of patients after surgery. It provides a structured framework that guides healthcare professionals in monitoring and supporting patient recovery. This SOP helps minimize risks and improve overall patient outcomes by standardizing care practices.
Which personnel are responsible for implementing the procedures outlined in post-operative care SOPs?
The responsibility for implementing post-operative care SOPs primarily lies with nurses, surgeons, and anesthesiologists. These healthcare professionals collaborate closely to monitor patient recovery and follow the detailed steps outlined in the SOP. Support staff may also assist in executing specific tasks as per their assigned roles.
What are the essential steps included in the initial assessment of a patient after surgery as per the SOP?
The initial assessment in post-operative care SOPs includes checking vital signs such as heart rate, blood pressure, and oxygen saturation. It also involves evaluating the patient's level of consciousness and pain management status. Immediate identification of any abnormalities or complications is critical for timely intervention.
How does the SOP address the documentation and communication of post-operative observations?
The SOP mandates thorough documentation and communication of all post-operative observations to ensure continuity of care. Healthcare providers are required to record vital signs, patient complaints, and any interventions performed in the patient's medical records. Clear communication between shifts and care teams is emphasized to prevent errors and promote effective recovery management.
What protocols are followed if post-operative complications arise, according to the SOP?
When post-operative complications arise, the SOP dictates immediate assessment and stabilization of the patient. It outlines specific protocols for notifying the surgical team and initiating emergency interventions if necessary. Documentation of the event and a review of intervention outcomes are also crucial components of the response protocol.
